What is Andrology: Everything You Need to Know
When we talk about men’s health, most people think of heart disease, weight, or fitness. Yet a man’s reproductive health is just as central to his overall well-being.
While gynaecology focuses on female reproductive health, andrology looks at the male half of the equation.
In this guide, we’ll break down exactly what andrology covers, why you might need an andrologist, and how simple lifestyle changes can boost fertility.
What is Andrology?
Andrology is the branch of medicine devoted to the study, diagnosis, and treatment of male reproductive health and fertility.
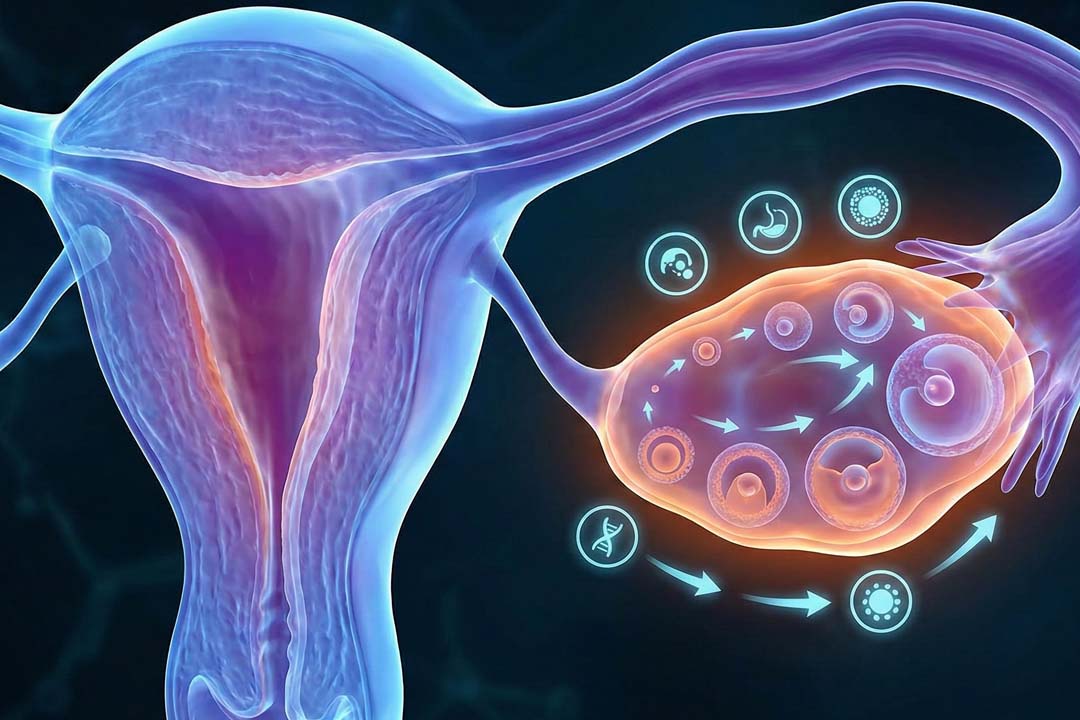
Andrology covers everything from sperm production in the testes to the delicate balance of hormones that drive libido.
It also investigates structural issues like varicoceles, hormonal problems such as low testosterone, and functional concerns including erectile dysfunction.
How is Andrology Different from Urology and General Medicine?
Andrology stays focused on reproduction, while urology covers the entire urinary tract. Urologists treat conditions of the kidneys, bladder, ureters, prostate, and male genitals. An andrologist, however, focuses on semen quality, hormone profiles, and male infertility.
Think of urology as the broad umbrella and andrology as the specialised area that deals specifically with male fertility and sexual function.
That focus means andrologists are trained to interpret semen reports, prescribe targeted hormone therapy, and offer fertility-saving surgeries.
What is the Role of an Andrologist?
The typical day involves physical exams, semen analysis, counselling, and sometimes microsurgery. Some common duties include:
- Physical exams check the testes, penis, and prostate for structural problems.
- Semen analysis looks at sperm count, movement (motility), and shape (morphology) to spot fertility problems.
- Hormone testing reveals low testosterone or other imbalances that affect sperm production or sex drive.
- Treatment plans might include medication for hormone support, procedures like varicocele repair, or assisted-reproductive techniques.
- Surgical work can range from vasectomy to more complex retrieval of sperm directly from testicular tissue.
When Should You Consider Booking an Appointment?
See an andrologist if you’ve tried to conceive for 12 months without success, face erectile problems, or notice changes in testicular size or libido.
Fertility issues are not just a female concern, male factors account for up to half of all cases where couples can’t conceive.
Early evaluation speeds up solutions and prevents needless stress. Even single men planning to store sperm ahead of cancer treatment or gender-affirming therapy can benefit from an andrology consult.
How does Semen Analysis Work and Why is it Important?
A semen test measures volume, count, motility, and shape to paint a clear picture of fertility potential.
You’ll be asked to abstain from ejaculation for 3–5 days, then collect the sample in a sterile cup. The lab keeps the sample warm and checks it under a microscope.
Typical targets (based on international guidelines) include 1.5 mL or more in volume, 15 million or more sperm per millilitre, at least 40 percent motile sperm, and at least 4 percent with ideal shape.
Falling short in one area doesn’t always mean infertility, but the pattern guides next steps such as lifestyle changes, medication, or advanced reproductive techniques.
What Treatments can an Andrologist Offer?
Options include medication, hormone therapy, minimally invasive surgery, and fertility preservation.
- Medication tackles infections and supports hormone balance.
- Hormone replacement corrects low testosterone or other endocrine gaps.
- Microsurgery can repair a varicocele or retrieve sperm when none appear in the ejaculate.
- Assisted reproduction like intracytoplasmic sperm injection (ICSI) uses even a single viable sperm to achieve pregnancy.
- Vasectomy and reversal give permanent or reversible contraception based on life plans.
- Sperm banking safeguards fertility before medical treatments that might harm the testes.
Do Lifestyle Choices Really Affect Sperm Quality?
Yes, smoking, excessive alcohol, obesity, and chronic stress can reduce count and motility, while good sleep, balanced diet, and exercise improve them.
Quitting tobacco, limiting alcohol, keeping a healthy weight, and managing stress all move the numbers in the right direction.
Even simple swaps like trading processed foods for antioxidant-rich fruits can help sperm DNA resist damage.
How is an Andrologist Different from a Sexologist?
An andrologist treats the medical side of male reproduction, whereas a sexologist focuses on sexual behaviour and relationships.
A sexologist may have medical or psychological training and often handles counselling for issues such as mismatched libido, sexual orientation questions, or relationship dynamics.
An andrologist, by contrast, runs lab tests, prescribes medicine, and performs surgery where needed.
The two specialists sometimes collaborate, especially when sexual dysfunction has both physical and psychological layers.
What Role Does Andrology Play in Family Planning?
It identifies male-factor problems early, offers sperm preservation, and supports assisted-reproduction strategies.
Men planning to start a family after 35, or those with risk factors such as varicoceles, can undergo a fertility check-up to avoid last-minute problems.
Andrology labs can freeze high-quality sperm for future use, giving couples greater freedom over timing. In cases where IVF or ICSI is required, the andrologist prepares the best possible sperm sample.
How Can You Prepare for an Andrology Visit?
List medications, record lifestyle habits, and follow abstinence instructions for semen tests. Arrive with your medical history, past surgeries, and any lab reports.
Wear comfortable clothing, stay hydrated, and follow any fasting or abstinence guidelines your clinic provides.
Conclusion
Whether you’re planning a family, grappling with erectile issues, or simply curious about your reproductive status, an andrologist can guide you with targeted tests and personalised care.
Early evaluation, healthy lifestyle choices, and open communication form the backbone of long-term reproductive wellness.
By acting today, you safeguard tomorrow’s possibilities for yourself, your partner, and any future family you hope to build.
Frequently Asked Questions
I’m 30 and healthy, should I get my fertility checked now?
If you plan to delay fatherhood for several years or have a lifestyle risk (smoking, high heat exposure at work), a baseline semen analysis can provide peace of mind and a point of comparison later.
Can stress lower my sperm count?
Chronic stress raises cortisol, which can interfere with testosterone production and impair sperm formation. Mindfulness, exercise, and adequate sleep help reverse the effect.
How long should I abstain before a semen analysis?
Most labs recommend 3–5 days without ejaculation. Shorter abstinence may cut volume, while longer periods can reduce motility.
Is erectile dysfunction always psychological?
Not always. Physical causes such as poor blood flow, diabetes, nerve damage, low testosterone are common. A thorough exam can pinpoint the source and guide treatment.
Does diet or supplementation improve sperm quality?
A diet rich in antioxidants, omega-3 fatty acids, zinc, and folate supports sperm health. Supplements help if blood tests reveal deficiencies, but food first is the rule.
Is a vasectomy reversible?
Yes, but success drops as years go by. If you might want children later, discuss sperm banking before the procedure.
How soon after a vasectomy can I stop using other contraception?
You’ll need follow-up semen tests usually at three and four months to confirm the absence of sperm. Until then, use alternative contraception.
About Us
AKsigen IVF is a premier center for advanced fertility treatments, with renowned fertility experts on our team. Specializing in IVF, ICSI, egg freezing, and other cutting-edge reproductive technologies, AKsigen IVF is committed to helping couples achieve their dream of parenthood. With personalized care and a patient-first approach, AKsigen IVF provides comprehensive fertility solutions under one roof.