Sonosalpingography vs HSG: Key Differences, Procedure & Accuracy
Many people first hear the terms sonosalpingography (often written as SSG/HyCoSy/HyFoSy) and HSG (hysterosalpingography) during an infertility work-up and wonder which test to pick.
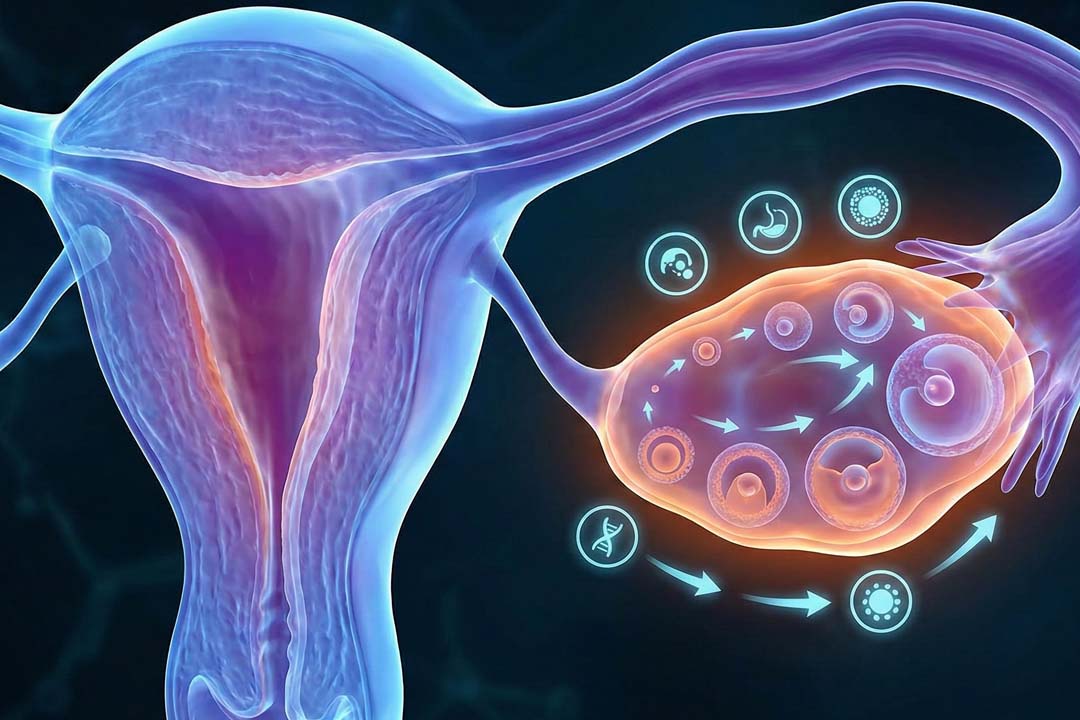
Both aim to check whether the fallopian tubes are open and to screen the uterine cavity for problems that could affect pregnancy.
The choice can depend on your medical history, access in your city, comfort with X-ray vs ultrasound, and whether your clinician needs extra detail about the tubes themselves.
What Each Test Actually Does?
Sonosalpingography (SSG/HyCoSy/HyFoSy) uses ultrasound with saline-air or foam contrast to watch fluid pass through the tubes; HSG uses low-dose X-ray (fluoroscopy) with an iodine-based dye to map the tubes and uterine cavity.
SSG avoids radiation and is typically performed by a gynecologist or sonologist using a transvaginal probe, while HSG is done in an X-ray suite using iodinated contrast that shows up on fluoroscopy.
- SSG = Sonosalpingography (umbrella term)
- HyCoSy = Hystero-salpingo-contrast sonography (saline + air or microbubble agents)
- HyFoSy = Hystero-salpingo-foam sonography (stabilized foam contrast for clearer tubal outlines)
Why Tubal Assessment Matters in an Infertility Work-up?
Blocked or damaged tubes can prevent egg and sperm from meeting; guidelines recommend assessing tubal patency based on the person’s risk profile.
For those with prior pelvic infection, endometriosis, or surgery, earlier testing is often advised; in lower-risk cases, a “visual patency test” (ultrasound- or X-ray-based) is commonly offered during evaluation.
How well do they find Blocked Tubes?
Both SSG/HyCoSy and HSG are reasonably accurate screening tests; modern evidence suggests HyCoSy can achieve sensitivity around ~89% and specificity around ~93%, while HSG’s performance varies and is often used as a reference screening tool before surgery.
Performance depends on operator experience, contrast used, and whether laparoscopy is used as the comparator. Several studies show HSG is good at detecting occlusion and characteristic tubal issues; contemporary reviews report HyCoSy’s accuracy approaching HSG when using optimized contrast (air–saline or foam) and 2D/3D imaging.
If your clinic regularly performs HyCoSy/HyFoSy, its detection of tubal patency/occlusion can be comparable to HSG, especially for a first-line, non-surgical screen.
Safety Profile and Comfort
SSG/HyCoSy/HyFoSy avoids radiation and typically uses saline/air or dedicated foam contrast, while HSG uses low-dose X-rays and iodinated dye; both are outpatient, and most people report crampy discomfort rather than severe pain.
Pre-procedure pain relief can help. Radiation from HSG is low, but X-ray exposure and iodine allergy need consideration; tell your clinician about infections or allergies ahead of time.
Foam contrast (HyFoSy) can enhance ultrasound visibility and may improve comfort and accuracy compared with older agents. Many centers now prefer foam because it remains visible in the tube lumen longer, outlining flow more clearly.
Which is better for Diagnostics?
HSG can better depict certain tube wall abnormalities that are inherently radiographic (e.g., salpingitis isthmica nodosa), whereas HyCoSy/HyFoSy excels when you want a radiation-free, clinic-based look at tubal patency and the uterine cavity in the same sitting. If your doctor suspects specific tubal pathologies or is considering tubal surgery, HSG’s fluoroscopic view can be informative.
Could the Test itself Improve Fertility?
Some evidence suggests that HSG, especially with oil-based contrast may transiently increase chances of pregnancy in the months following the test, possibly by flushing minor debris; the effect is not guaranteed and remains debated.
Patient education resources and systematic reviews note a short-term uptick in fertility after HSG in some groups, though it shouldn’t be seen as a treatment for significant tubal disease.
When are the Tests Performed?
Both tests are typically scheduled in the early follicular phase (after bleeding stops, before ovulation) to avoid interfering with a potential early pregnancy and to minimize infection risk. Clinics may prescribe a prophylactic antibiotic based on individual risk. Mild spotting and cramping for a day or two are common; severe pain or fever are reasons to call your provider.
HyCoSy accuracy: Recent analyses report pooled sensitivity ~89% and specificity ~93% for tubal patency against surgical comparators when performed with modern protocols.
HSG value: widely used as a first-line screen; fluoroscopic views can characterize occlusion and typical tubal pathologies and inform surgical planning.
Safety: HSG uses low-dose X-ray; adverse events are uncommon for both tests when standard infection precautions are followed.
Costs in India
Typical out-of-pocket ranges (and why they vary):
- HSG: Around ₹2,000–₹7,000 in many centers (some lists quote up to ~₹8,000+ depending on city, imaging suite charges, consumables, and whether anesthesia is used).
- SSG/HyCoSy/HyFoSy: Around ₹3,000–₹7,000 for standard setups (foam contrast or 3D/4D mapping may cost more; some quotes run higher depending on facility).
Always ask what’s included (scan, disposables, medications, and the consult to explain results) and confirm the final payable amount at your clinic in your city.
Radiation vs No Radiation
Choose SSG/HyCoSy/HyFoSy if you want a radiation-free first look; choose HSG if radiographic detail of the tubes is important or if your clinician prefers fluoroscopy to guide next steps. Either way, the dose with HSG is low and complications are uncommon, but radiation-free options are attractive for many.
How to Interpret the Results?
A “patent” tube means the contrast was seen exiting the tube; “delayed spill” or “sluggish flow” can reflect mild spasm or partial narrowing; “no spill” suggests a block that may need confirmation or further evaluation.
Your doctor will look at both tubes and the uterine cavity (polyps, fibroids, adhesions) and then align the plan with your age, ovarian reserve, semen analysis (including the IUI post-wash sperm count if you’re proceeding to IUI), and overall timeline.
When is Laparoscopy still Needed?
If a noninvasive test shows an abnormality and management hinges on precise anatomy or if endometriosis/adhesions are suspected your clinician may recommend diagnostic laparoscopy with dye as the definitive test and potential treatment in one sitting.
Noninvasive tests are excellent screens but don’t treat disease; laparoscopy remains the gold standard when surgical correction is on the table.
Frequently Asked Questions
Which hurts less between SSG/HyCoSy or HSG?
Most people describe both as crampy rather than truly painful; pre-procedure analgesics help. HyCoSy avoids the sting some feel with iodinated dye, and foam contrast can improve comfort and visibility. Experiences do vary.
Is there radiation with SSG/HyCoSy?
No. SSG/HyCoSy uses ultrasound. HSG uses low-dose X-rays; exposure is small and considered safe when appropriately indicated.
Can these tests increase my chances of conceiving?
Sometimes. Studies note a short-term rise in pregnancy rates after HSG, particularly with certain contrast media, possibly due to a flushing effect. It’s a bonus, not a guarantee.
Which test is better if I have a known iodine allergy?
SSG/HyCoSy is generally preferable since it doesn’t use iodinated contrast. Always discuss your allergy history with your clinician first.
How soon after the test can I try to conceive or plan IUI?
Usually the same cycle, once spotting/cramps settle. Your clinician will time IUI/ovulation induction based on your cycle monitoring and, if relevant, the IUI post-wash sperm count. (Clinical practice guidance perspective.)
If my HyCoSy is normal, do I still need HSG?
Usually no; if HyCoSy shows clear bilateral spill and a normal cavity, many clinicians proceed with treatment. A second test may be suggested if symptoms/history point to specific tubal disease better characterized on X-ray.
Conclusion
Choose the test that best aligns with your history and the decisions it will guide. If you prefer a radiation-free, clinic-based screen with real-time ultrasound, SSG/HyCoSy/HyFoSy is compelling. If your team wants fluoroscopic detail or you’re considering tubal surgery, HSG remains a robust first-line map. The most important step is to discuss the pros and cons with your clinician, clarify how the result will change your plan (IUI vs IVF), and make sure cost and comfort fit your needs.
About Us
AKsigen IVF is a premier center for advanced fertility treatments, with renowned fertility experts on our team. Specializing in IVF, ICSI, egg freezing, and other cutting-edge reproductive technologies, AKsigen IVF is committed to helping couples achieve their dream of parenthood. With personalized care and a patient-first approach, AKsigen IVF provides comprehensive fertility solutions under one roof.