What is Recurrent Pregnancy Loss?
Losing a pregnancy is more common than many people realize, and most single losses are random and not a sign of a long-term problem. Recurrent pregnancy loss (RPL) is when pregnancy losses happen more than once. Medical groups define it slightly differently.
In practice, doctors usually start an evaluation after two losses because that’s when the odds of an underlying issue begin to rise.
The aim of a work-up is to look for patterns which can be genetic, anatomical, hormonal, or immune-related, that can be corrected or managed before the next pregnancy.
Even when no cause is found, many people still go on to have a healthy baby with time, support, and careful follow-up.
How Common is it and What is the Outlook?
Miscarriage affects roughly 10–20% of known pregnancies. RPL is less common, about 1% of people of reproductive age.
The most important message is prognosis: even after multiple losses, the chance of a future live birth is often 50–70% (or higher) depending on age and cause, especially with supportive care and targeted treatment when a cause is found.
Causes of Recurrent Pregnancy Loss
It is important to understand the causes of recurrent pregnancy loss for a better action plan. The causes can be as follows:
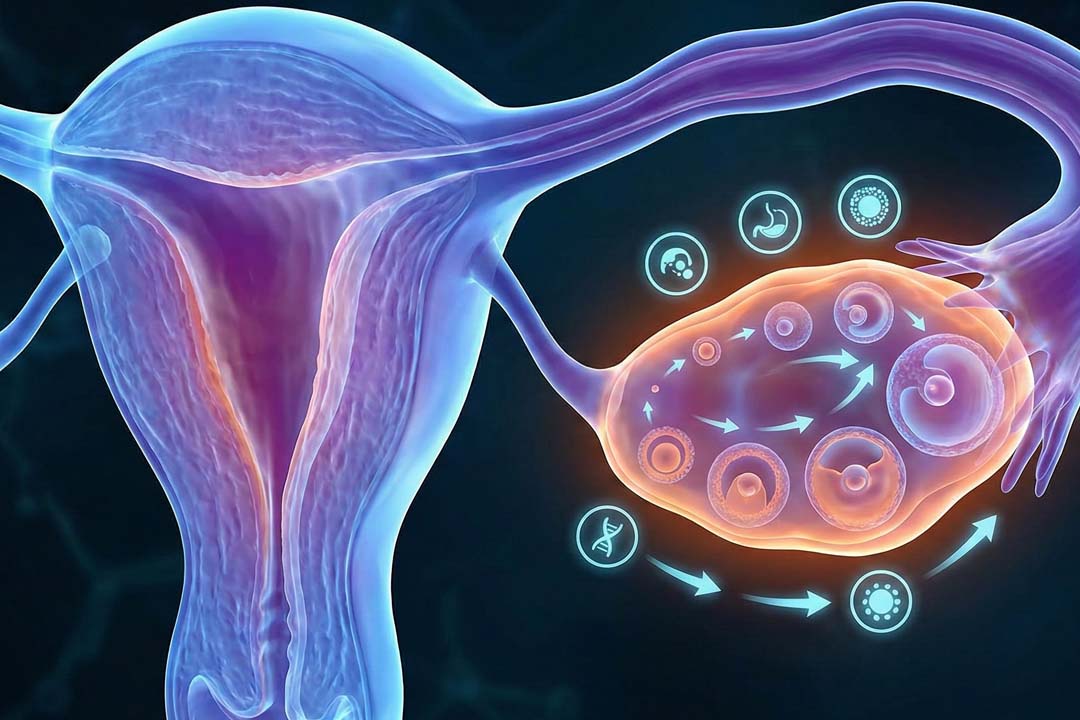
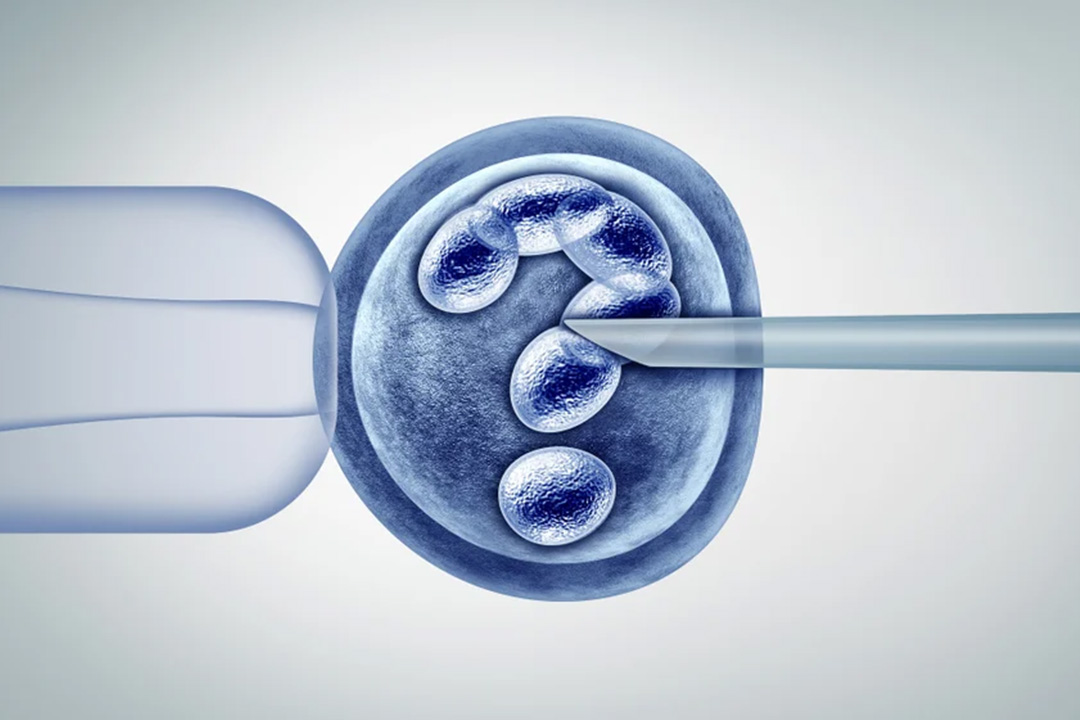
Genetic and Chromosomal Factors
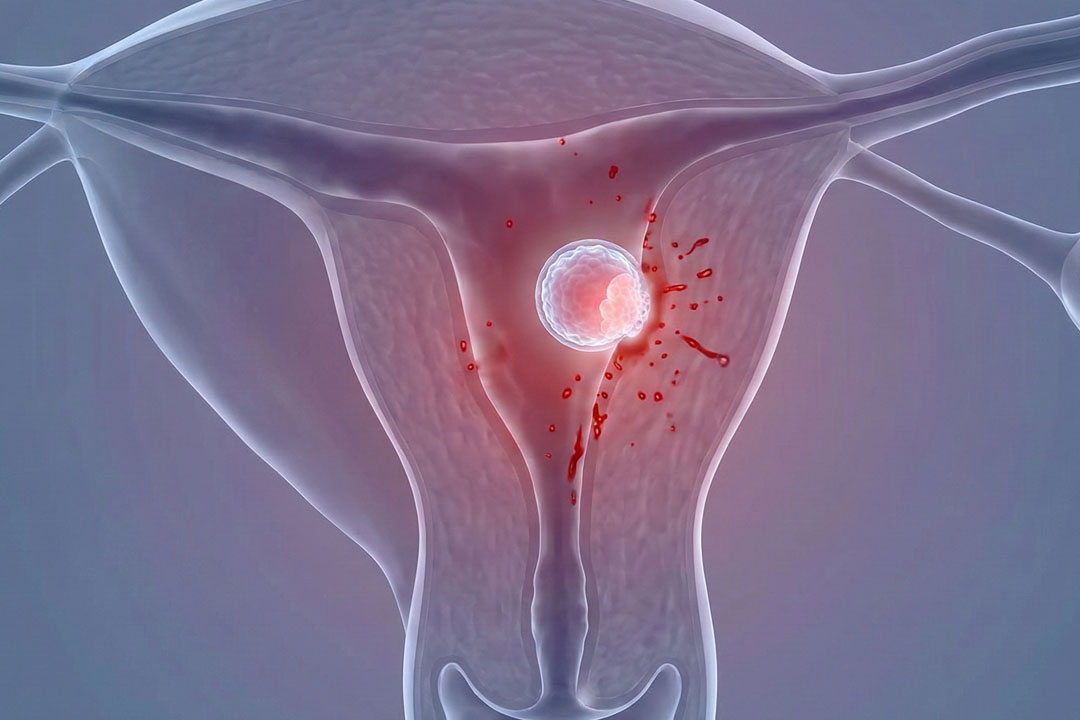
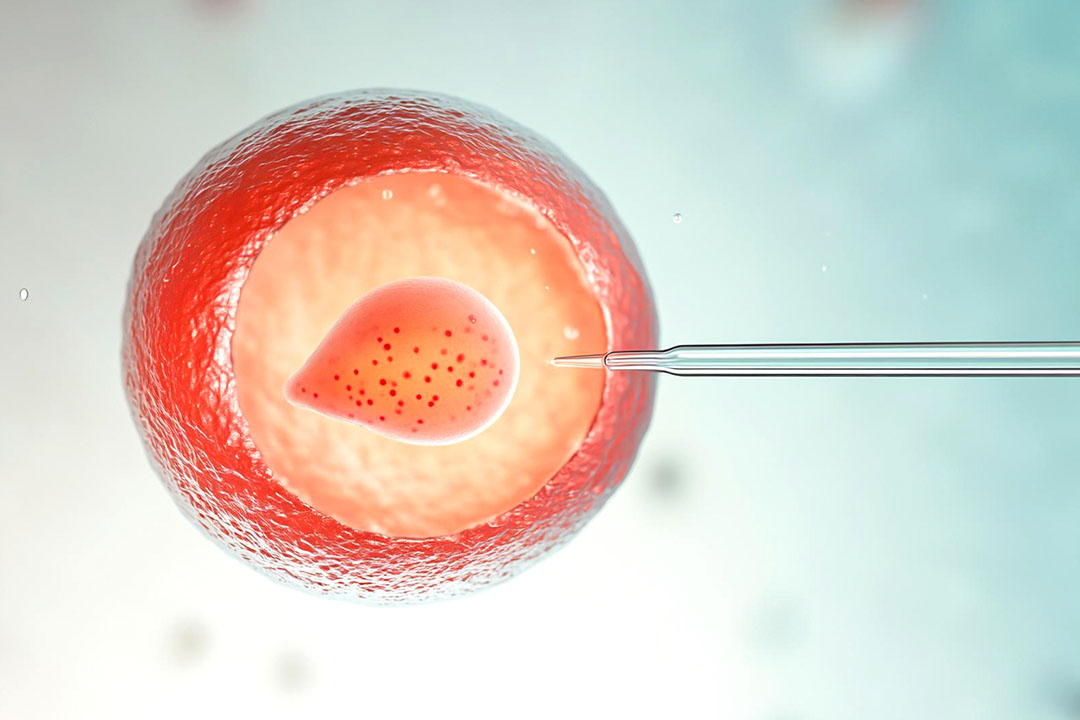
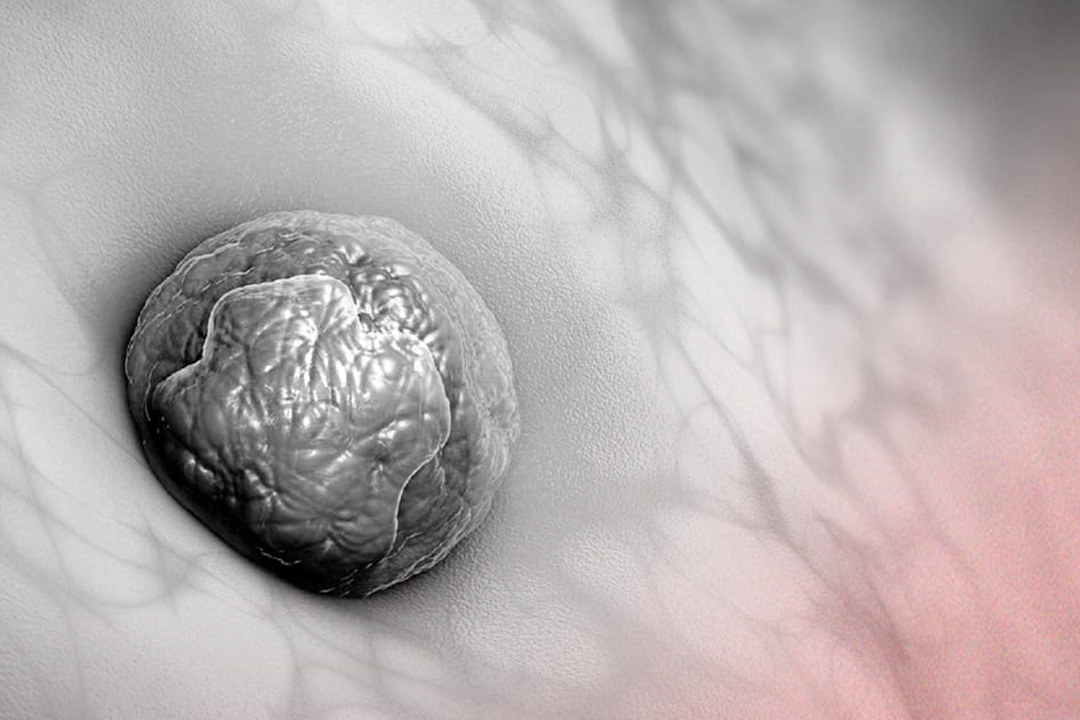
The single most frequent reason for early losses is a chromosomal error in the embryo. These are usually “de novo” changes that happen at conception and are more likely as egg age increases.
Chromosomal issues are detected in a large share of first-trimester losses, and maternal age strongly influences this risk.
When losses repeat, doctors may test the pregnancy tissue (when available) and sometimes the parents’ chromosomes to look for a balanced rearrangement (e.g., a translocation) that can raise the risk of unbalanced embryos.
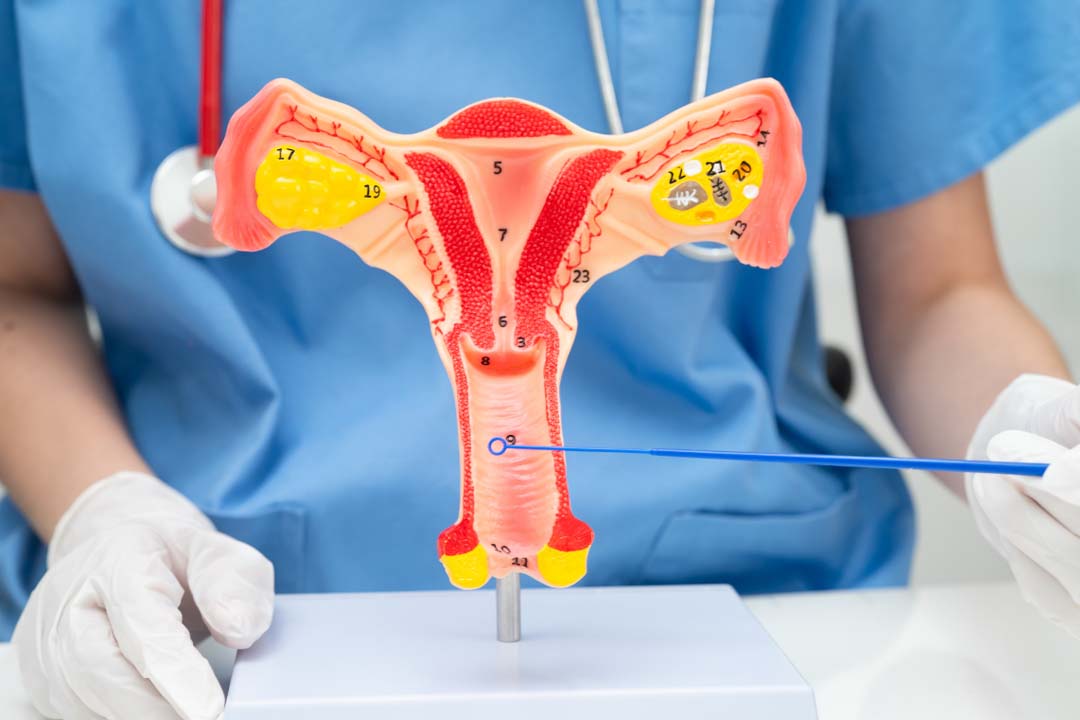
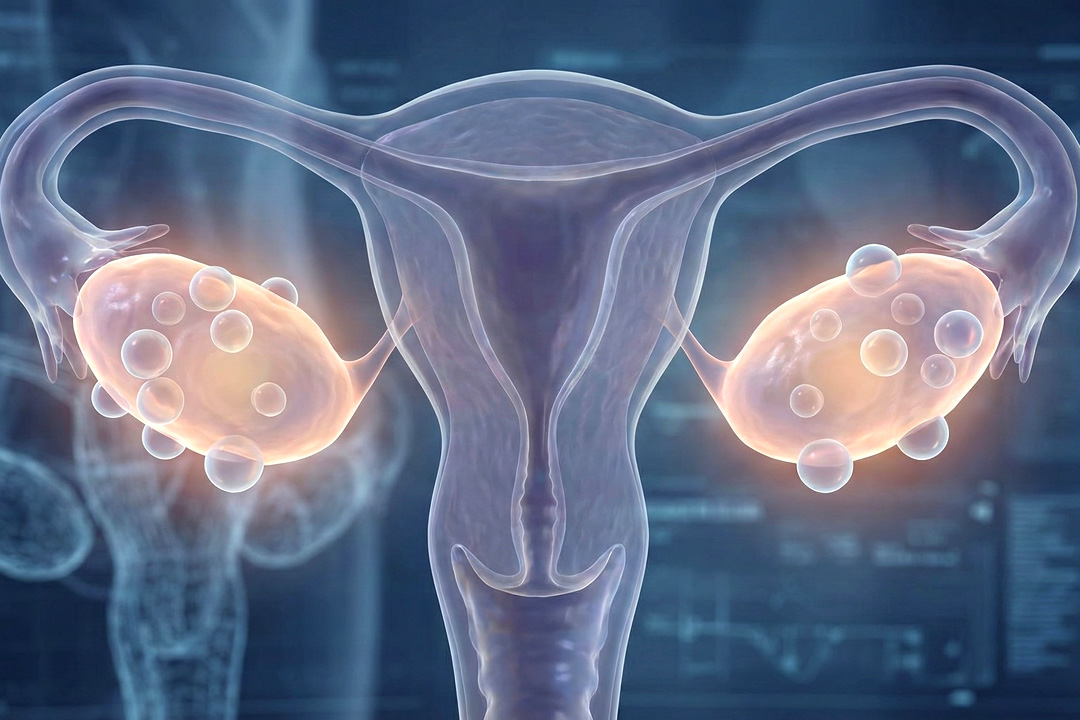
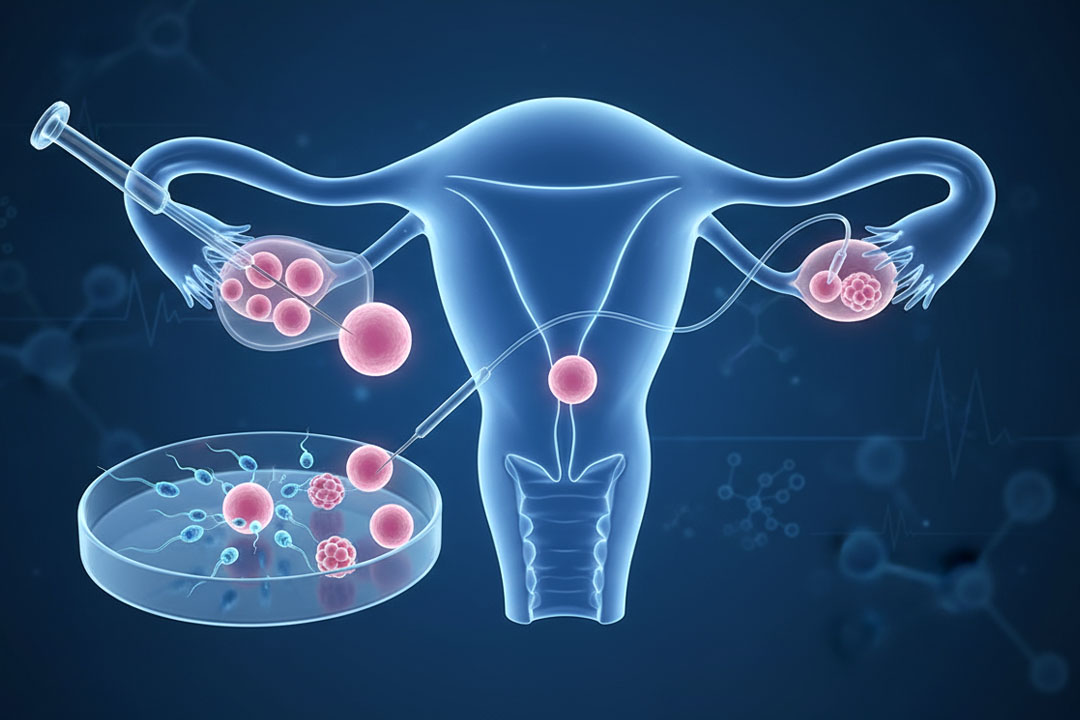
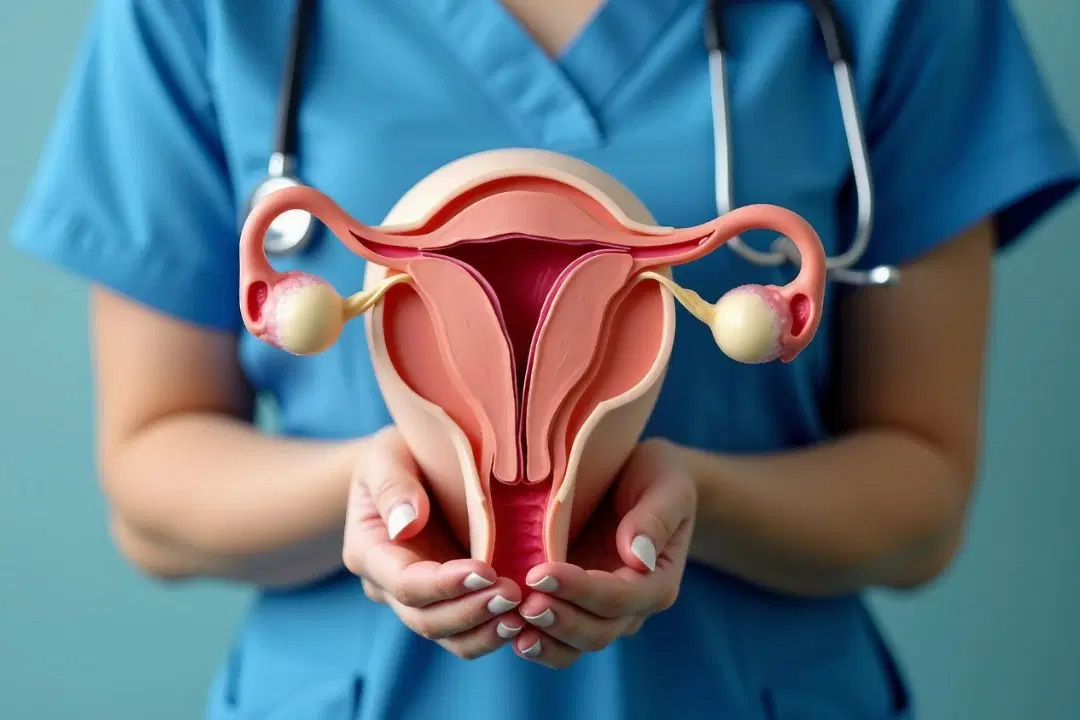
Uterine (anatomical) Factors
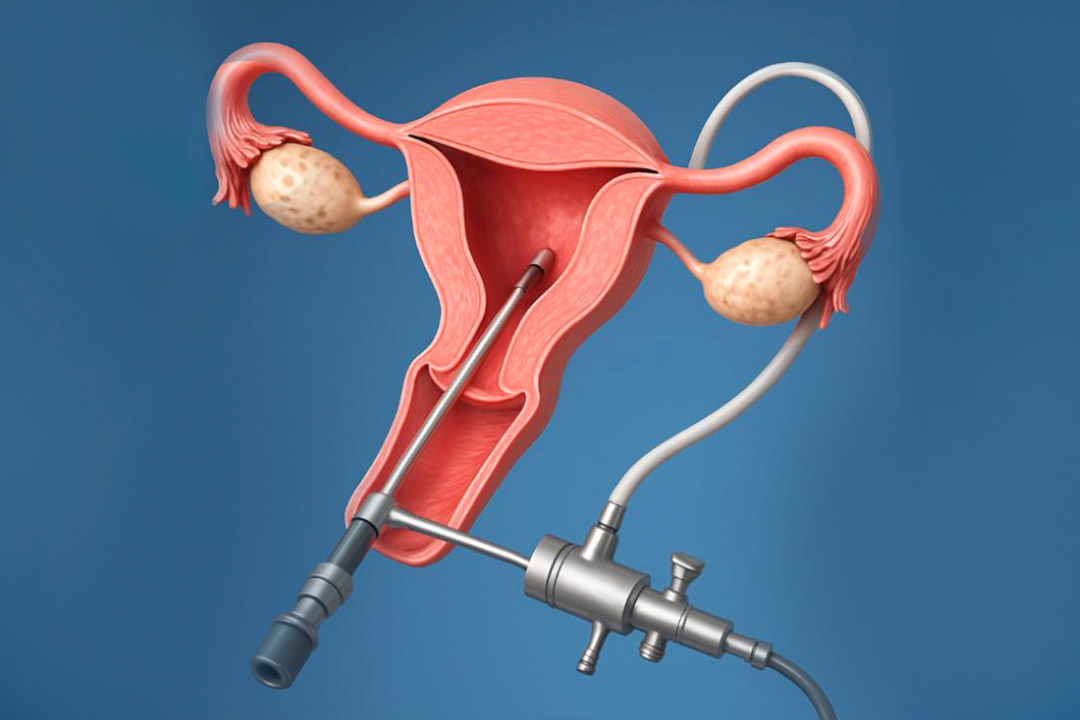
The structure of the uterus matters. A septate uterus (a wall dividing the cavity) is the congenital abnormality most linked with miscarriage; fibroids or polyps that distort the cavity and intrauterine adhesions can also interfere with implantation and growth.
Imaging, which usually uses saline-infusion sonography, 3D ultrasound, hysteroscopy, or HSG, maps the cavity to guide treatment. RCOG’s 2023 guideline supports considering hysteroscopic septum resection in
women with RPL, ideally in centers that audit outcomes.
Hormonal and Metabolic Factors
Thyroid disease, poorly controlled diabetes, and high prolactin levels can increase risk and are routinely addressed.
Recent ESHRE guidance recommends TSH and thyroid peroxidase (TPO) antibody screening in RPL; if overt hypothyroidism is present, treatment with levothyroxine is indicated. Good glycemic control and tailored management of other endocrine issues are standard parts of care.
Immune and Clotting Factors (especially APS)
A well-established cause is antiphospholipid syndrome (APS), an autoimmune condition defined by clinical criteria (e.g., pregnancy morbidity) plus persistent antiphospholipid antibodies (lupus anticoagulant, anticardiolipin IgG/IgM, and anti-β2-glycoprotein I IgG/IgM).
When APS is confirmed, treatment in pregnancy with low-dose aspirin and heparin improves outcomes. Without APS, routine anticoagulation is not recommended for unexplained RPL.
Infections
Chronic or acute infections are unlikely to explain repeated early miscarriages in most cases. Outside specific clinical clues (e.g., second-trimester loss suggestive of cervical/infectious pathways), routine “infection panels” are not recommended by major guidelines.
Lifestyle and Age
Smoking, heavy alcohol use, high caffeine intake, and obesity are all modifiable risks. RCOG advises BMI 19–25, smoking cessation, limiting alcohol, and keeping caffeine <200 mg/day.
Age matters because aneuploidy risk rises with oocyte age. Addressing weight, diet, and exposure belongs in every care plan.
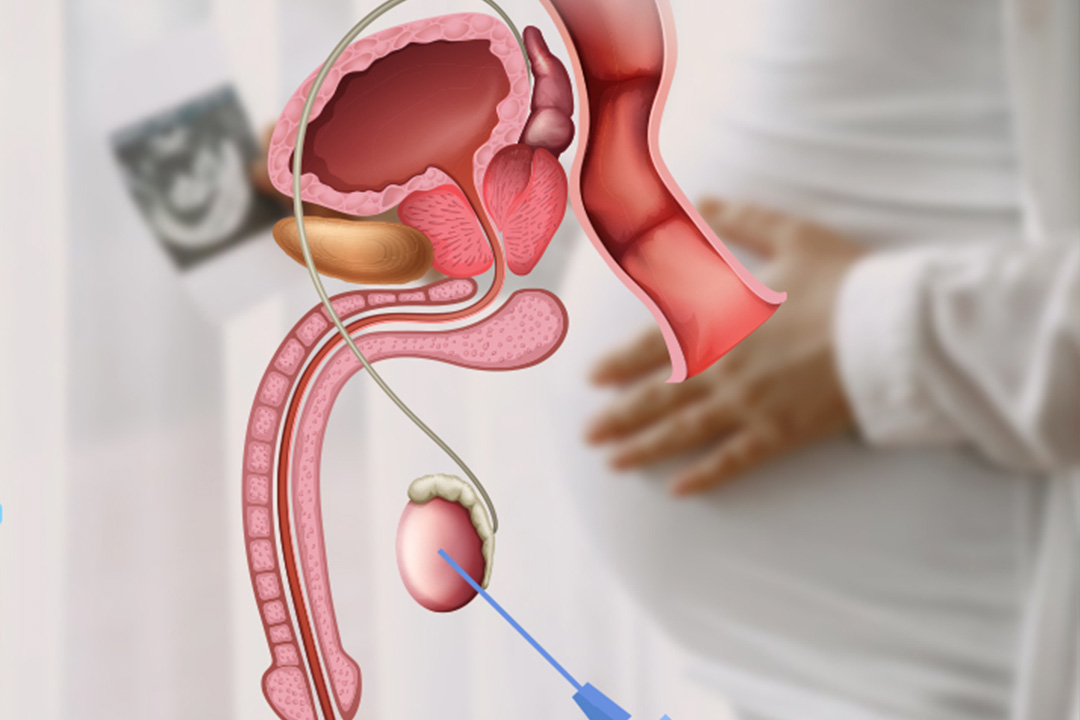
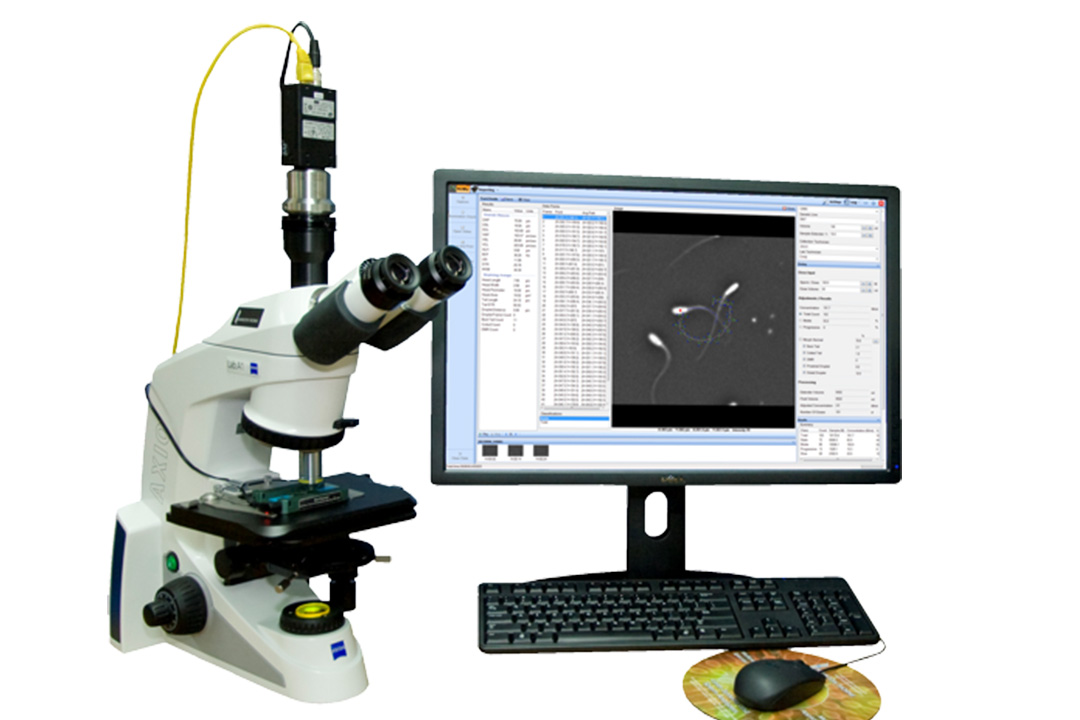
Male Factors
Standard semen testing is often normal in RPL. Some studies explore sperm DNA fragmentation, but most guidelines do not recommend it as routine because evidence linking it to targeted, effective treatment remains limited.
Recurrent Pregnancy Loss: What the Guidelines Recommend
Guidelines for recurrent pregnancy loss (key points)
- Definition & timing: Start evaluation after two clinically recognized losses.
- Core evaluation: Detailed history and exam; uterine cavity imaging (SIS/3D ultrasound or hysteroscopy); APS testing (LA, aCL IgG/IgM, anti-β2GPI IgG/IgM); targeted endocrine work-up (e.g., TSH, diabetes, prolactin as indicated). Consider parental karyotypes when products of conception suggest a rearrangement or when history is suggestive.
- What not to do routinely: Broad infectious screens, inherited thrombophilia panels, and “immune” panels without a clear indication.
- Treatment examples: Manage the specific cause (e.g., metroplasty for a septum; optimize thyroid/diabetes; aspirin + heparin only for APS). Provide early pregnancy support and monitoring in subsequent pregnancies.
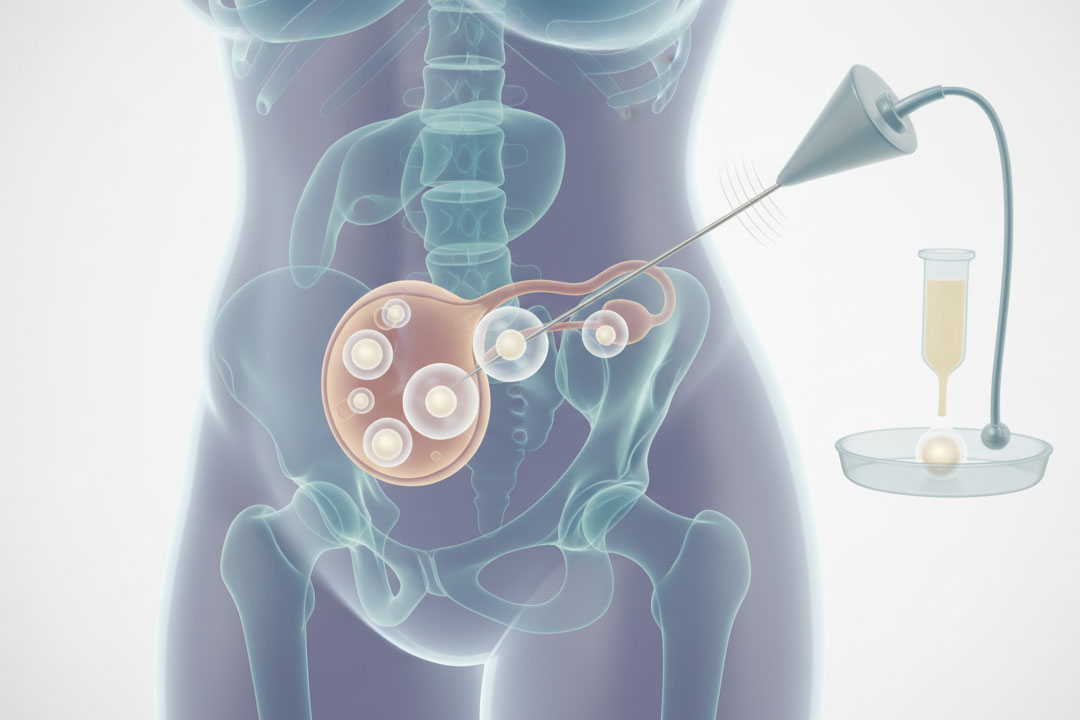
Genetic Studies
- Products of conception (if obtainable) using karyotype or chromosomal microarray can clarify whether aneuploidy caused the loss.
- Parental karyotypes in selected cases (e.g., repeated aneuploid losses or a structural rearrangement on tissue testing).
- Routine inherited thrombophilia panels, broad infection screens, natural killer cell assays, or cytokine panels, these don’t change care for most patients.
Treatment For Recurrent Pregnancy Loss
Treat the specific problem when you find one, and support early pregnancy closely either way.
- APS: Use low-dose aspirin plus heparin in pregnancy (and for a period postpartum per rheumatology/obstetric guidance). This combination lowers miscarriage risk in APS; it is not advised for unexplained RPL.
- Uterine septum or cavity-distorting lesions: Hysteroscopic surgery (septum resection; polypectomy; targeted fibroid removal) can improve the environment for implantation and growth.
- Endocrine disorders: Normalize thyroid function (treat overt hypothyroidism), optimize diabetes control, and treat hyperprolactinemia when present.
- Progesterone: Consider vaginal micronized progesterone in women with early pregnancy bleeding and a history of previous miscarriages; routine use for all unexplained RPL is not supported.
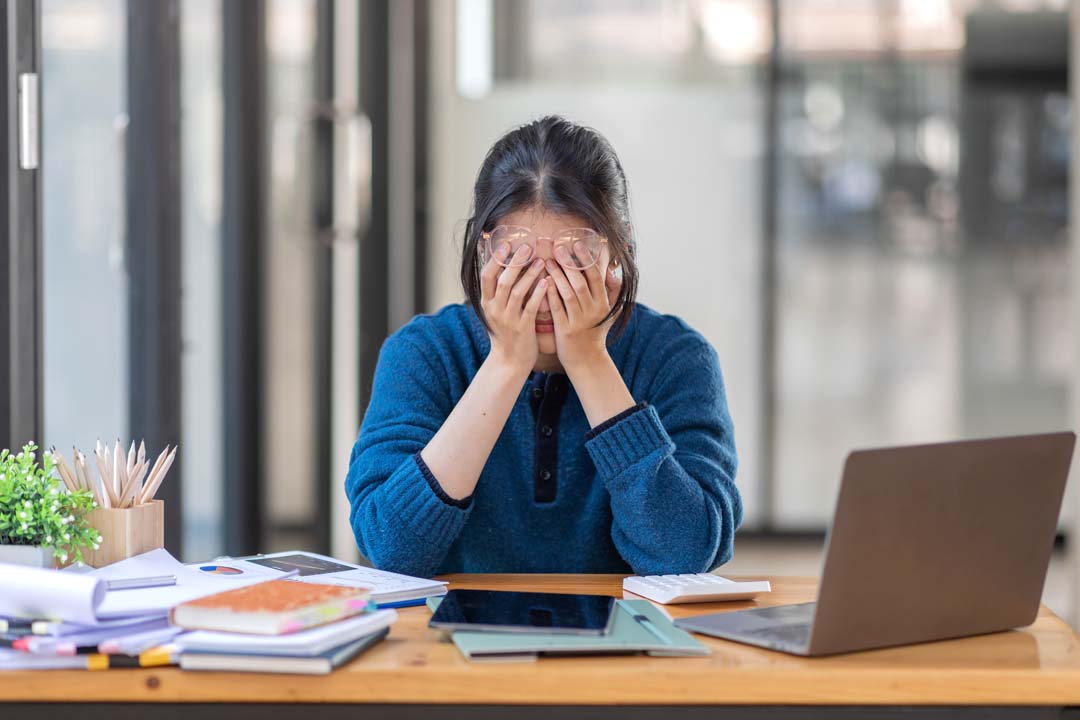
- Supportive (“TLC”) care: Early and frequent contact, reassurance, and serial ultrasounds/β-hCG can meaningfully reduce anxiety and are associated with better continuation rates in some cohorts.
Immunotherapy for Recurrent Pregnancy Loss
Outside of APS (which is treated with aspirin + heparin), most “immunotherapies” remain experimental.
IVIG, intralipid infusions, lymphocyte immunization (LIT), steroids without a defined autoimmune diagnosis, G-CSF, and anti-TNF agents have been studied, but major guidelines do not recommend them for unexplained RPL due to inconsistent benefit, cost, and potential risks.
Some newer studies report signals in highly selected subgroups, but these are not practice-changing yet. If considered at all, it should be within research protocols or with full counseling about uncertain benefit.
Frequently Asked Questions
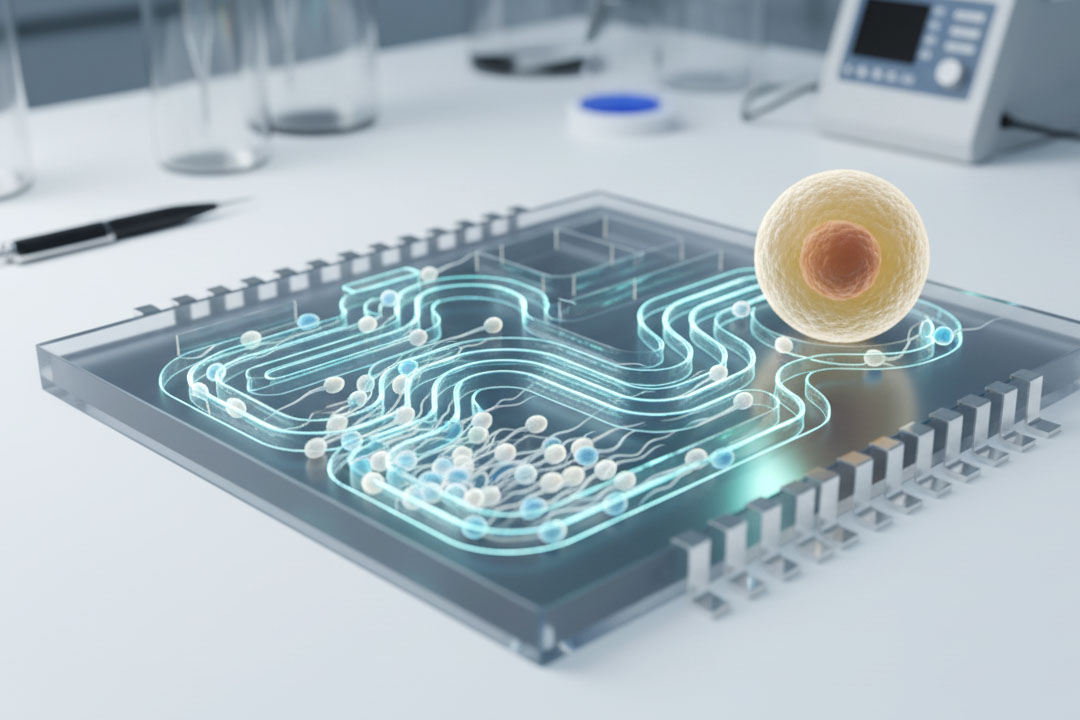
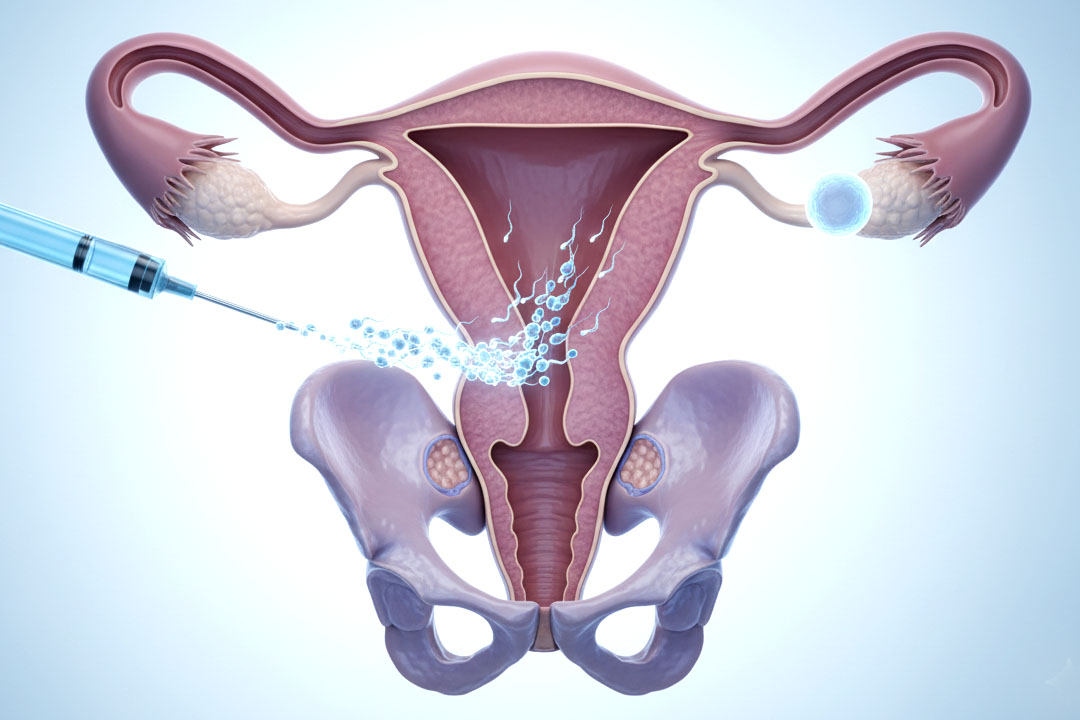
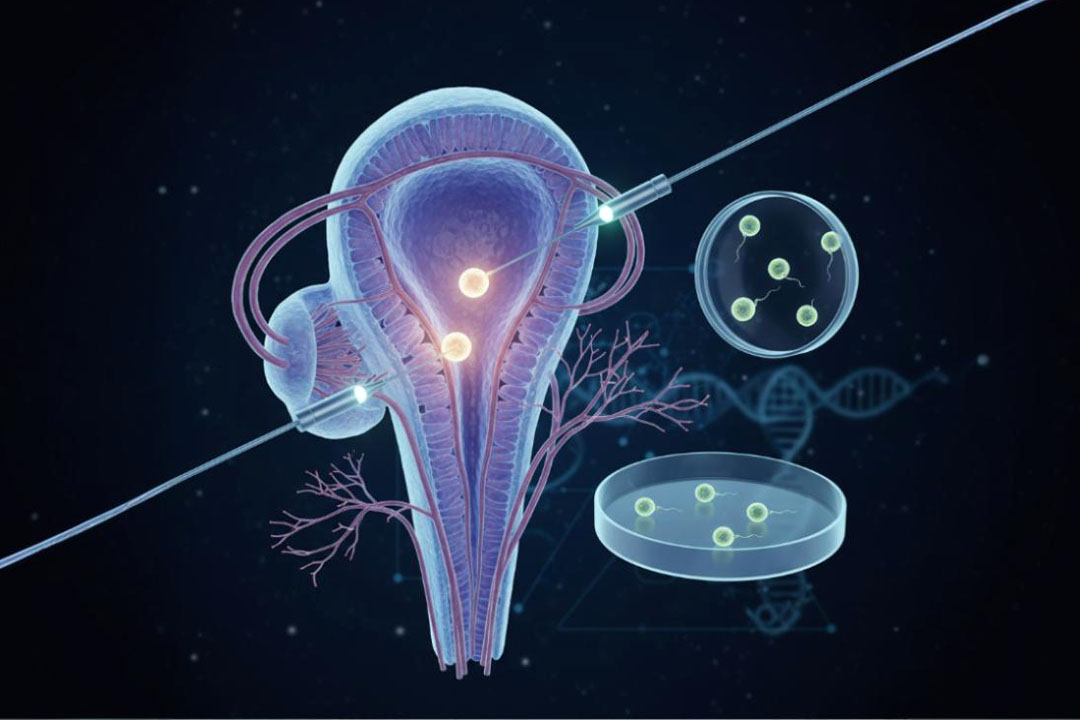
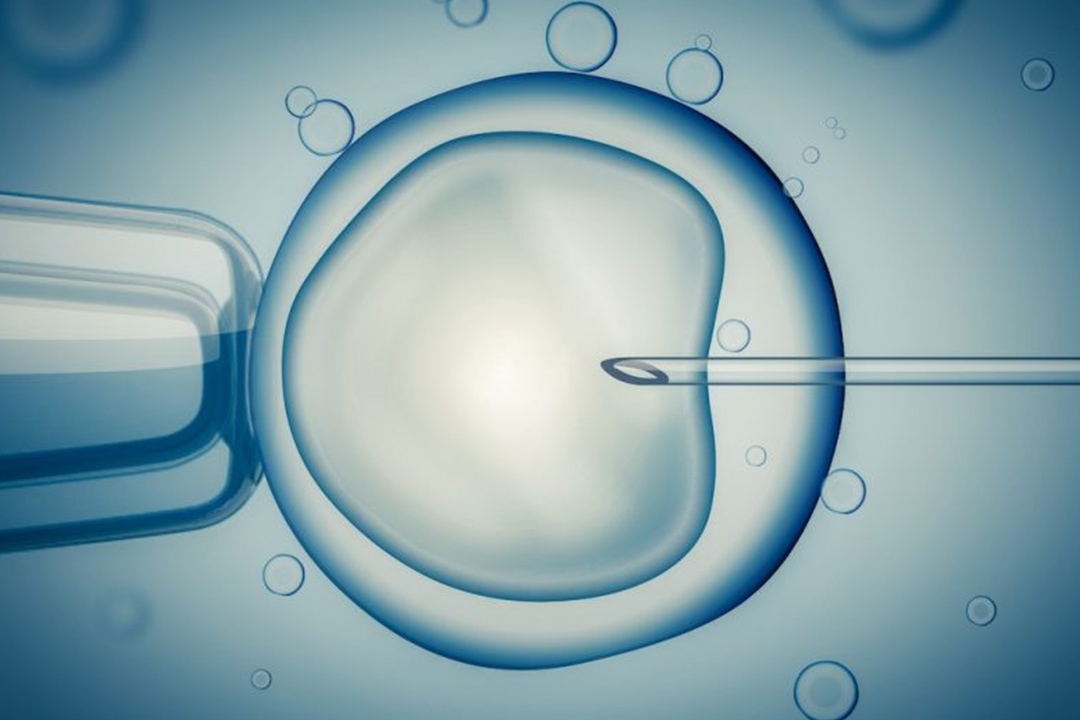
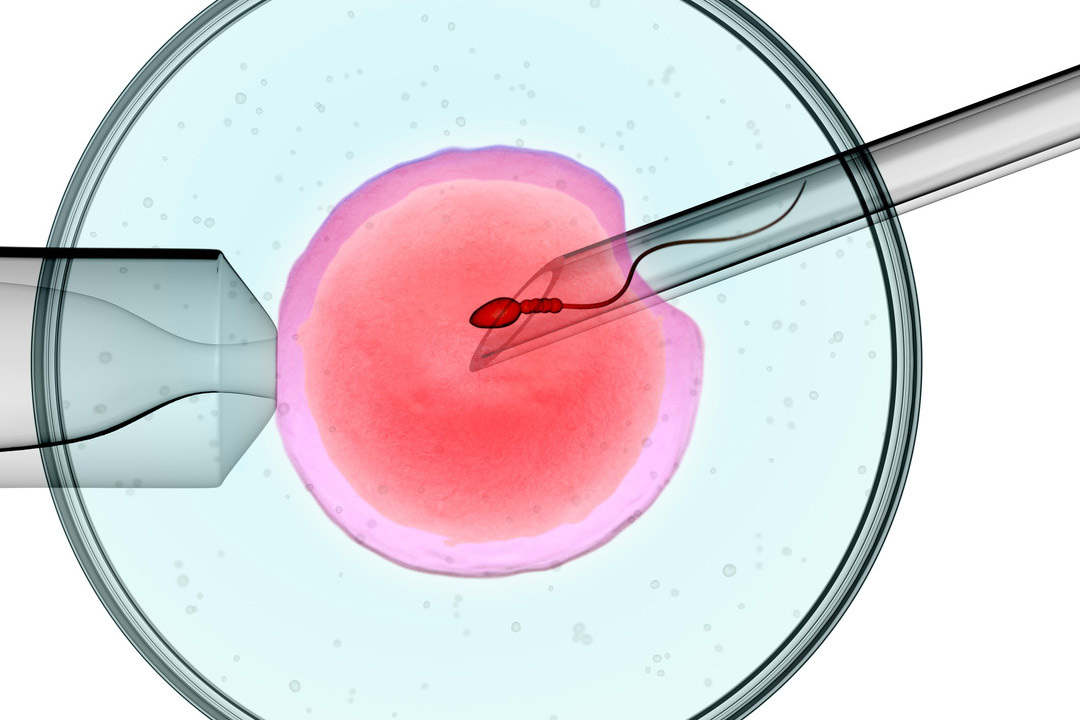
Is IVF automatically needed after recurrent miscarriages?
No. IVF is not a default treatment for RPL. It’s considered when there’s a specific reason such as a parental chromosomal rearrangement where embryo testing (PGT) might help select a chromosomally balanced embryo. Even then, guidelines caution that PGT-A does not clearly improve live-birth rates for unexplained RPL and carries costs and risks. Many people conceive naturally after evaluation and supportive care.
When should I start testing?
After two losses. That’s the point at which ACOG and many clinics suggest beginning a structured evaluation. RCOG still defines RPL as three losses but supports starting earlier when clinically appropriate.
Does progesterone help prevent another loss?
Sometimes, under specific circumstances. Evidence supports vaginal progesterone for women who have bleeding in early pregnancy and a history of prior miscarriage(s). Routine progesterone for all with unexplained RPL (without bleeding) hasn’t shown a clear benefit.
Which tests really matter for recurrent pregnancy loss?
Core tests include uterine imaging, APS antibody panel, and targeted endocrine labs (TSH ± TPO Ab, diabetes markers, prolactin when indicated). Genetic analysis of pregnancy tissue, when available, is informative. Broad infection screens, inherited thrombophilia panels, NK cell tests, and cytokine panels are not part of a standard work-up.
What can I change right now to avoid pregnancy loss?
Aim for a healthy BMI, stop smoking, limit alcohol, and keep caffeine under 200 mg/day. Manage thyroid disease and diabetes, review medications/exposures, and start a prenatal vitamin with folic acid while planning your next pregnancy.
What are my chances next time?
Often better than you fear. Depending on age and cause, many see 50–70% (or more) live-birth chances in subsequent pregnancies, even when no specific cause is found. Early, compassionate monitoring helps.
Conclusion
Recurrent pregnancy loss is devastating, but it’s also workable. Identify it early (after two losses), look carefully for treatable causes, and support the next pregnancy from the start. For APS, aspirin plus heparin is evidence-based.
For uterine factors, targeted hysteroscopic surgery can help and for endocrine issues, optimize control. In many cases, simple changes and attentive care are enough. Most importantly, the outlook is often positive with a realistic plan and support, many go on to have the healthy pregnancy they’ve been hoping for.
About Us
AKsigen IVF is a premier center for advanced fertility treatments, with renowned fertility experts on our team. Specializing in IVF, ICSI, egg freezing, and other cutting-edge reproductive technologies, AKsigen IVF is committed to helping couples achieve their dream of parenthood. With personalized care and a patient-first approach, AKsigen IVF provides comprehensive fertility solutions under one roof.