Microchip Method in IVF: Advanced Sperm Selection Technique

Advances in reproductive medicine have developed fast over the last decade, bringing couples fresh hope via safer and more successful fertilization therapies. One such development is the microchip approach in in vitro fertilization (IVF), a new technique that selects the healthiest sperm in a manner that closely resembles natural fertilization in an effort to increase embryo quality.
While many people find success with traditional sperm-selection methods, there are certain drawbacks. Repeated centrifugation is one technique that can put sperm cells under more stress and, in certain situations, cause DNA damage. These restrictions may have an impact on treatment results for couples dealing with infertility that cannot be explained, poor embryo development, or excessive sperm DNA fragmentation.
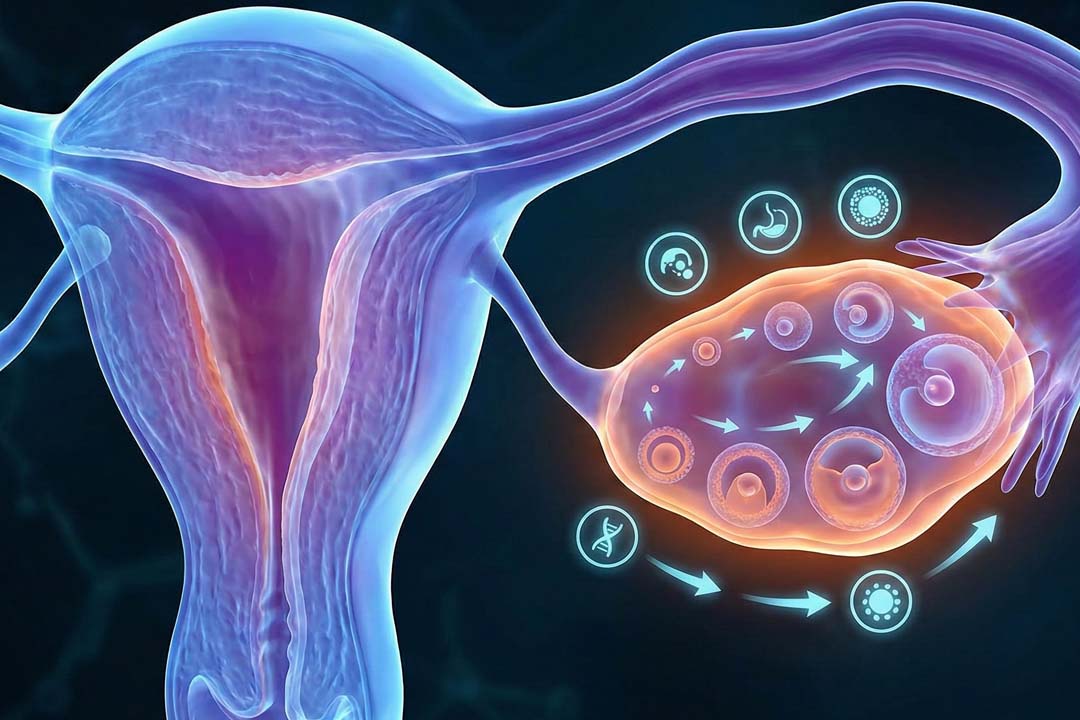
The microchip technique brings in a softer, more physiology-friendly approach. Instead of depending on powerful mechanical forces, this approach moves sperm via microscopic channels designed to simulate the environment of the female reproductive system.
Only the strongest, most motile, and most genetically intact sperm successfully transit through the microchannels, similar to how sperm normally move toward an egg in the body. Because of this, the method has gained attention for its potential to improve embryo development, especially by day 5 (blastocyst stage), and increase the chances of a successful pregnancy.
This article explores how the microchip method works, its advantages, who it may benefit the most, and what patients can expect during treatment.
Microchip Method in IVF
The microchip method is a sperm-selection technology used before IVF or ICSI. It is built on a simple but powerful idea: healthy sperm naturally move better, faster, and more consistently than damaged or poorly functioning sperm.
How the method works in simple terms
Instead of spinning a semen sample in a centrifuge which can generate oxidative stress and sometimes harm the DNA inside sperm cells, the microchip system allows sperm to swim freely through a set of narrow channels carved into a small chip.
These channels are designed to imitate the uterus, cervix, and vaginal pathway. Strong, healthy sperm move through these structures smoothly, while sperm with weak movement or DNA issues are naturally filtered out.
At the end of the channel, the healthiest sperm accumulate in a small reservoir, from where they are collected for use in IVF or ICSI.
Why Conventional Sperm Preparation Has Limitations
Traditional sperm-processing methods have long relied on techniques such as:
- Centrifugation
- Density-gradient separation
- Swim-up method
While these techniques often work well, they involve mechanical force. In some cases, these movements can lead to the production of reactive oxygen species (ROS), which can harm sperm DNA. Sperm with compromised DNA are often linked to poor embryo development, lower success rates in IVF, and higher chances of miscarriage.
Furthermore, conventional methods do not fully mimic natural sperm selection. In the body, only a small percentage of sperm reach the egg after overcoming many barriers. Some of these barriers help filter out sperm with genetic problems.
The microchip method strengthens this nature-inspired filtering without exposing sperm to heavy handling.
How the Microchip Method Mimics Natural Fertilization
In the female reproductive system, sperm undergo multiple stages of selection:
- Vaginal entry: Only motile sperm move forward.
- Cervical filtering: Sperm with poor structure or low movement are removed.
- Uterine and tubal navigation: Only the healthiest sperm continue progressing.
The microchip system recreates this selection journey in a controlled laboratory setup.
Key Features of the Microchip Environment
- Micro-sized channels that resemble the narrow passages sperm travel through naturally.
- Flow characteristics that encourage forward progression similar to how sperm move toward the egg.
- No centrifugation, so sperm are not exposed to high external pressure.
- A natural “race” where only the fittest sperm reach the end.
Because the sperm “compete” and move forward using their natural ability, the final sample tends to contain sperm with:
- High motility
- Intact DNA
- Better morphology
- Lower oxidative stress
- Higher fertilizing potential
These features are especially important for couples undergoing ICSI, where a single sperm cell is injected into an egg.
Benefits of the Microchip Method
This method provides several benefits, for instance:
1. Lower chance of DNA damage
Since the process does not rely on centrifugation, the risk of damaging sperm DNA through oxidative stress is reduced.
2. More physiologically natural selection
Sperm are not chosen manually or under external pressure; they must swim on their own strength, closely resembling natural selection.
3. Better embryo development potential
Studies have shown improved embryo quality, particularly noticeable at the blastocyst stage (day 5), because healthier sperm contribute to better cell division and growth.
4. Helps patients with high sperm DNA fragmentation
Men with elevated DNA fragmentation often face repeated IVF failures. The microchip method helps isolate sperm with the least damage.
5. Useful in unexplained infertility
Couples with repeated unsuccessful attempts may benefit because the technique filters out subtle sperm defects often missed in standard testing.
6. Gentle and less invasive for sperm
Without spinning or layering, the method reduces the stress placed on sperm and keeps the selection environment stable.
7. Suitable for IUI and IVF/ICSI treatments
Although it is mainly associated with IVF, the method can also improve sperm quality before intrauterine insemination.
Who May Benefit From the Microchip Method?
This method can be helpful for many fertility patients, but it is especially suitable in the following cases:
Patients undergoing IUI
Using higher-quality sperm may improve chances of fertilization during an insemination cycle.
Individuals with high sperm DNA fragmentation
If sperm DNA fragmentation tests show elevated levels, the microchip method may help isolate healthier sperm for ICSI.
Couples with recurrent pregnancy loss
When the reason for miscarriage is unclear, poor sperm DNA integrity could be one of the underlying factors. Selecting sperm with intact DNA helps reduce this risk.
People experiencing repeated IVF failure despite good eggs
Sometimes eggs are healthy, but embryos do not grow well. In these cases, subtle sperm issues may be responsible, making microchip selection helpful.
Couples with unexplained infertility
When no cause is identified, improving sperm selection can potentially solve hidden male-factor issues.
How the Microchip Method Improves IVF Outcomes
While no sperm-selection technique can guarantee success, using sperm with intact DNA and strong motility plays a major role in:
- Fertilization rates
- Blastocyst formation
- Embryo quality
- Implantation potential
- Lower miscarriage risk
By decreasing stress on sperm and relying on natural mobility, the microchip technique increases the likelihood of choosing sperm with higher growth ability. Many clinics that utilize this procedure report better day-5 embryo growth than typical preparation techniques.
Limitations of the Method
While helpful, the technique is not a cure-all. Some limitations include:
- It cannot fix severe sperm production problems.
- Very low sperm count samples may still require conventional methods.
- Embryo development depends on both egg and sperm quality.
Frequently Asked Questions
1. Is IVF with the microchip method suitable for someone who is 30?
Yes. IVF at age 30 generally has good success rates, and using the microchip method may support better sperm selection if there are male-factor concerns or repeated failed cycles.
2. Does the microchip method increase IVF success?
It can improve embryo quality and blastocyst development by selecting healthier sperm, which may increase success rates, especially in cases of DNA fragmentation or unexplained infertility.
3. Does the method hurt or damage sperm?
No. It is actually gentler than centrifugation-based techniques and reduces the risk of DNA damage.
4. What is the cost of the microchip method in India?
The cost typically ranges between ₹10,000 to ₹25,000 depending on the clinic and the type of IVF cycle.
5. Can this method be used for ICSI?
Yes. In fact, microchip-selected sperm are often used directly for ICSI because they tend to have better motility and lower DNA fragmentation.
6. Can microchip sperm selection help reduce miscarriage risk?
It may help in cases where poor sperm DNA integrity contributes to pregnancy loss.
7. Will it help if the male partner has normal semen analysis?
Even when the standard test appears normal, hidden DNA issues can exist. In such cases, microchip selection may still improve embryo development.
8. Is it useful for couples with one failed IVF cycle?
Yes. Many couples with at least one failed attempt use this method to improve their next cycle.
9. Is the procedure painful?
The sperm preparation procedure is performed in the lab and is not painful for the patient.
10. Does this method replace all other sperm selection techniques?
No, but it is an advanced option that may provide better results in selected cases.
Conclusion
The microchip approach in IVF is a potential innovation that takes science closer to nature's initial use for picking the healthiest sperm. This method, which relies on the sperm's natural motility and avoids harsh preparation processes, aids in the identification of sperm with superior DNA integrity and higher fertilization potential.
For couples dealing with unexplained infertility, repeated IVF failure, or sperm DNA fragmentation, the microchip approach provides an extra layer of support that may increase embryo quality and overall treatment results.
As reproductive treatments advance, tools like these assist make IVF more tailored, successful, and patient-friendly. While it may not be required for every couple, it is a useful tool for many and represents continual advances in reproductive health.
About Us
AKsigen IVF is a premier center for advanced fertility treatments, with renowned fertility experts on our team. Specializing in IVF, ICSI, egg freezing, and other cutting-edge reproductive technologies, AKsigen IVF is committed to helping couples achieve their dream of parenthood. With personalized care and a patient-first approach, AKsigen IVF provides comprehensive fertility solutions under one roof.